What is CP@clinic?
CP@clinic is an innovative, evidence-based chronic disease prevention, management, and health promotion program that seeks to:
Improve older adults’ health and quality of life, and reduce their social isolation
Better connect older adults with primary care, and community resources
Reduce the economic burden of avoidable 911 calls by older adults
- Locations accessible to large numbers of in-need individuals
- To date, mostly in the common rooms of subsidized housing buildings
- Now expanding to other settings such as shelters and community centers
Maria Attends A Typical CP@clinic Session
Maria is 75 and lives alone in her apartment. She has been diagnosed with high blood pressure and uses a walker. Most of her family lives out of town so she doesn’t have many visitors. She leaves her apartment once a week to run errands and do her laundry. She notices the new CP@clinic poster in her apartment lobby and decides to go to a CP@clinic session.
Navigate the banner below to follow Maria through her CP@clinic session.
Facts & Figures
CP@clinic is an evidence-based program, meaning that it was derived and informed by research. CP@clinic’s impact was first evaluated in a pilot project and then later in a large research trial and produced very positive results!
CP@clinic Reduces 911 Calls by 19-25%

The average number of ambulance calls per month was significantly lower in buildings that had CP@clinic compared to control buildings without CP@clinic, across multiple communities.
- 19% less calls in the CP@clinic multi-site randomized controlled trial1
- 22% less calls in 3 intervention buildings in Hamilton, ON2
- 25% less calls in the CP@clinic pilot study3
This reduction in 911 calls may allow for the reallocation of ambulances for those who are in greater need
CP@clinic Improves Quality of Life

Those who attended CP@clinic showed significant improvements in:
- self-care (washing & dressing themselves)1
- ability to engage in “usual activities”1,2 , and
- pain and discomfort1
There was a significant QALY gain ranging from 0.05 - 0.15 for those attending CP@clinic sessions1,2
QALYs: Quality-Adjusted Life Years
Improved quality of life can lead to older adults developing better coping skills and increased resiliency
**Quality-adjusted life years (QALYs) are a common measure used to assess whether a drug, intervention, or program can increase or decrease the number of years in good health lived by participants. QALY is defined as one year of life lived in perfect health.4
CP@clinic Reduces Chronic Disease Risk

Blood pressure:
- For participants who had a high BP at their 1st CP@clinic session, 40.5% had their BP normalize after attending several CP@clinic sessions1
- For participants who had a high BP at their 1st CP@clinic session, their average BP decreased significantly by 5.0 mmHg systolic and 4.8 mmHg diastolic after the 2nd and 4th sessions. This decrease was sustained across 10 or more visits.2
Diabetes Risk:
- 50 of 63 or 79% of participants were identified as high risk of developing diabetes in the next 10 years.2
- There was an improvement in participants’ diabetes risk after several CP@clinic sessions.1,2 This demonstrates the positive effects of the tailored health education of CP@clinic in this setting.
CP@clinic Empowers Participants

CP@clinic participants are actively engaged in goal setting. Participants set goals for themselves based on their chronic disease risk factors enabling them to take charge of their health
“It keeps you involved in your own health management also right. It brings awareness of health issues.” -CP@clinic Participant 5
Connects to Primary Care

- 715 of 794, or 90% of residents who attended CP@clinic were provided with health education and directed towards their family physician for chronic disease risks1
- 95%, or 755 of 794 participants had regular reports with their CP@clinic assessment results faxed to participants’ primary care providers potentially enabling them to receive optimal care1
Cost Effective
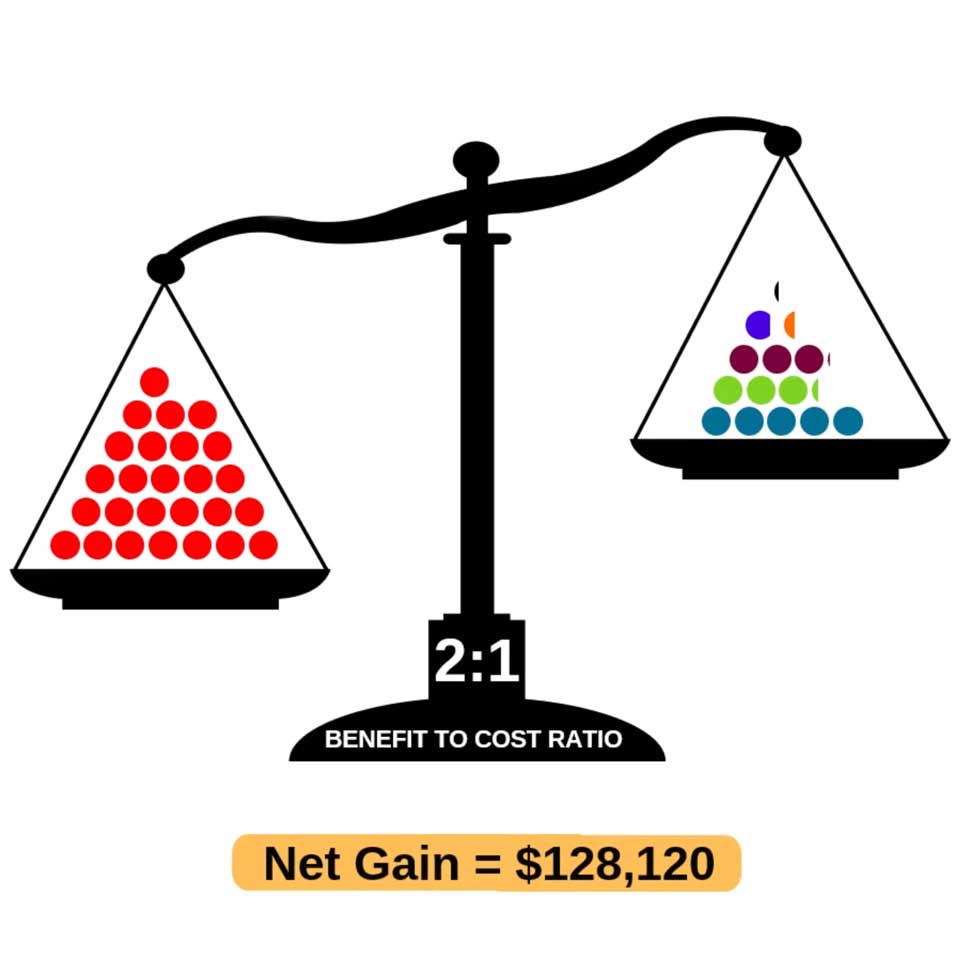
- CP@clinic is Proven to be Cost-effective. Benefit to Cost Ratio of 2:1 - For every $1 spent on the CP@clinic Program, the Emergency Care System sees $2 in benefits6
- Using data from the CP@clinic Randomized Controlled Trial in 13 social housing buildings with 1461 residents6
- Watch the Cost-Effectiveness of CP@clinic Infographic Video for more information.
- Agarwal G, Angeles R, Pirrie M, McLeod B, Marzanek F, Parascandalo J, Thabane L. (2019). Reducing 9-1-1 emergency medical service calls by implementing a community paramedicine program for vulnerable older adults in public housing in Canada: A multi-site cluster randomized controlled trial. Prehospital Emergency Care. 23(5): 718-729.
- Agarwal G, Angeles R, Pirrie M, McLeod B, Marzanek F, Parascandalo J. (2018). Evaluation of a Community Paramedicine Health Promotion and Lifestyle Risk Assessment Program in Seniors Living in Social Housing Buildings: A Cluster Randomized Trial. CMAJ. 190(21): E638-E647
- Agarwal G, Angeles R, Pirrie M, Marzanek F, McLeod B, Parascandalo J, Dolovich L. (2017). Effectiveness of a community paramedic-led health assessment and education initiative in a seniors' residence building: the Community Health Assessment Program through Emergency Medical Services (CHAP-EMS).BMC Emergency Medicine. 17(8): 1-8.
- Cape, J.D., Beca, J.M., and Hoch, J.S. (2013). Introduction to Cost-Effectiveness Analysis for Clini-cians. University of Toronto Medical Journal, 90(3). Accessed from http://healtheconomics.utoronto.ca/wp-content/uploads/1493-2720-2-PB3.pdf
- Brydges M, Agarwal G, Denton M. (2016). The CHAP-EMS health promotion program: a qualitative study on participants' views of the role of paramedics. BMC Health Service Research. 16(435): n/a.
- Agarwal G, Pirrie M, Angeles R, Marzanek F, Thabane L, O'Reilly D. Cost-effectiveness analysis of a community paramedicine programme for low-income seniors living in subsidised housing: the community paramedicine at clinic programme (CP@clinic) BMJ Open 2020;10:e037386. doi: 10.1136/bmjopen-2020-037386
Infographics
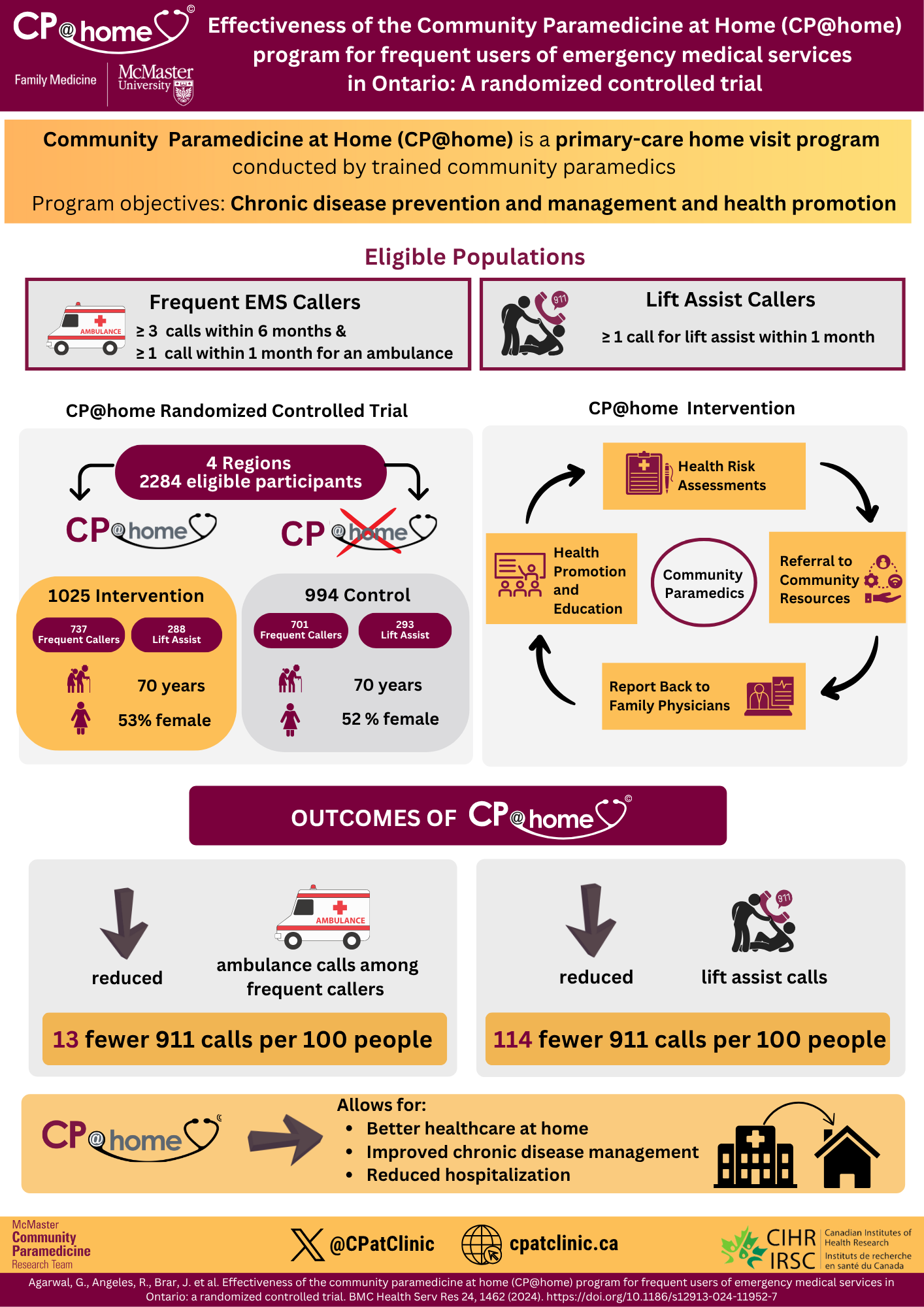
Effectiveness of the Community Paramedicine at Home (CP@home) program for frequent users of emergency medical services in Ontario: A randomized controlled trial
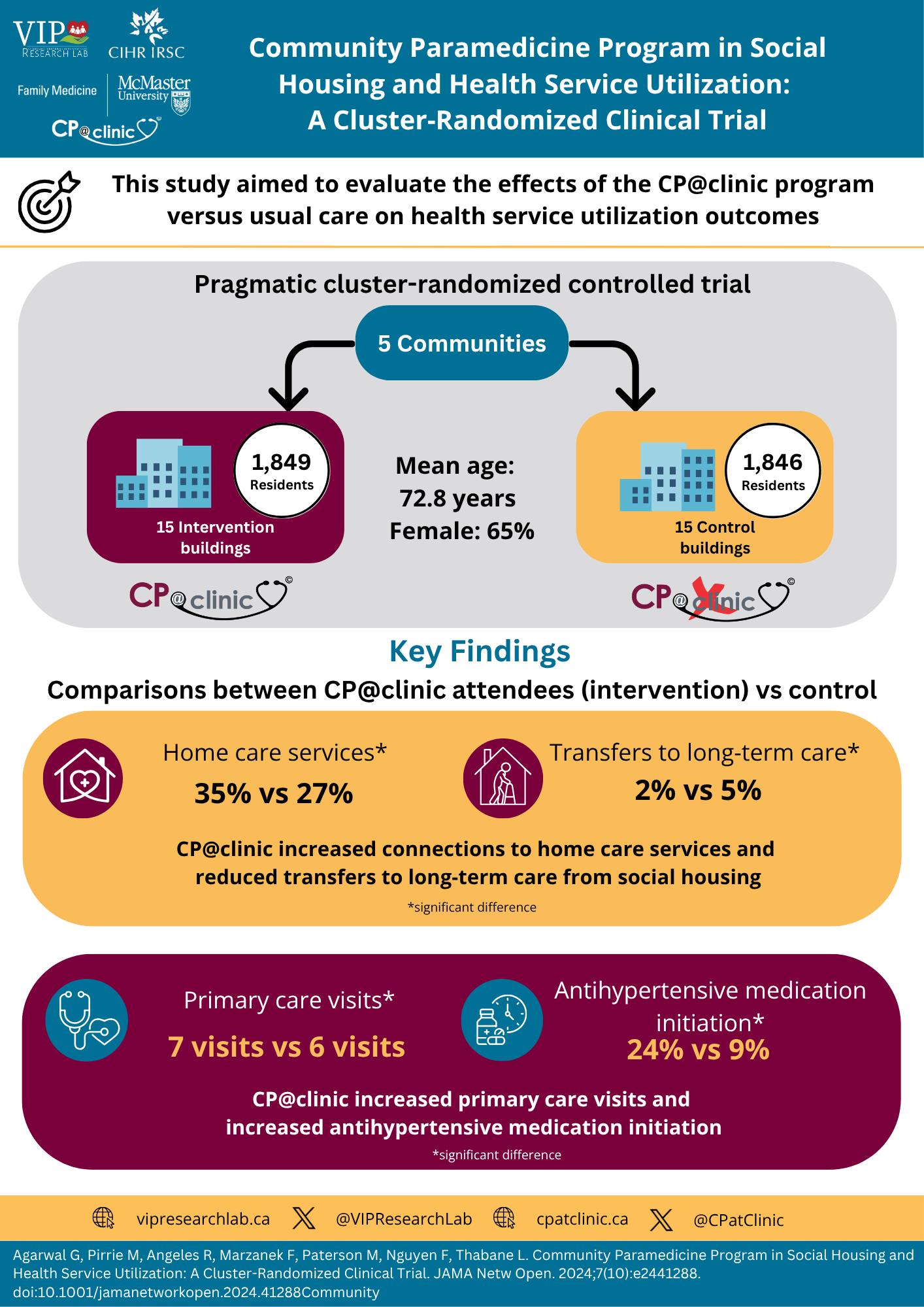
Community Paramedicine Program in Social Housing and Health Service Utilization: A Cluster-Randomized Clinical Trial
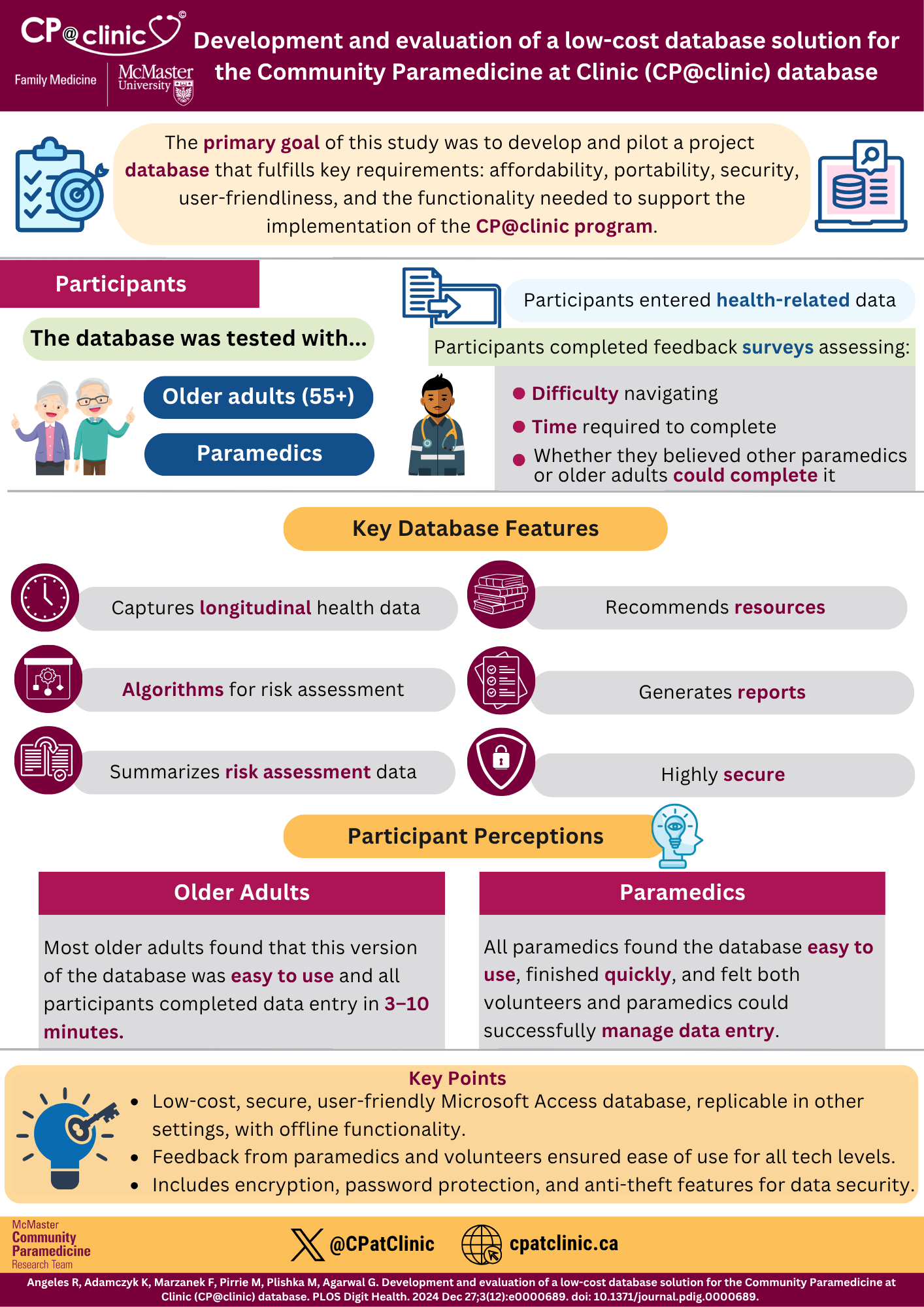
Development and evaluation of a low-cost database solution for the Community Paramedicine at Clinic (CP@clinic) database
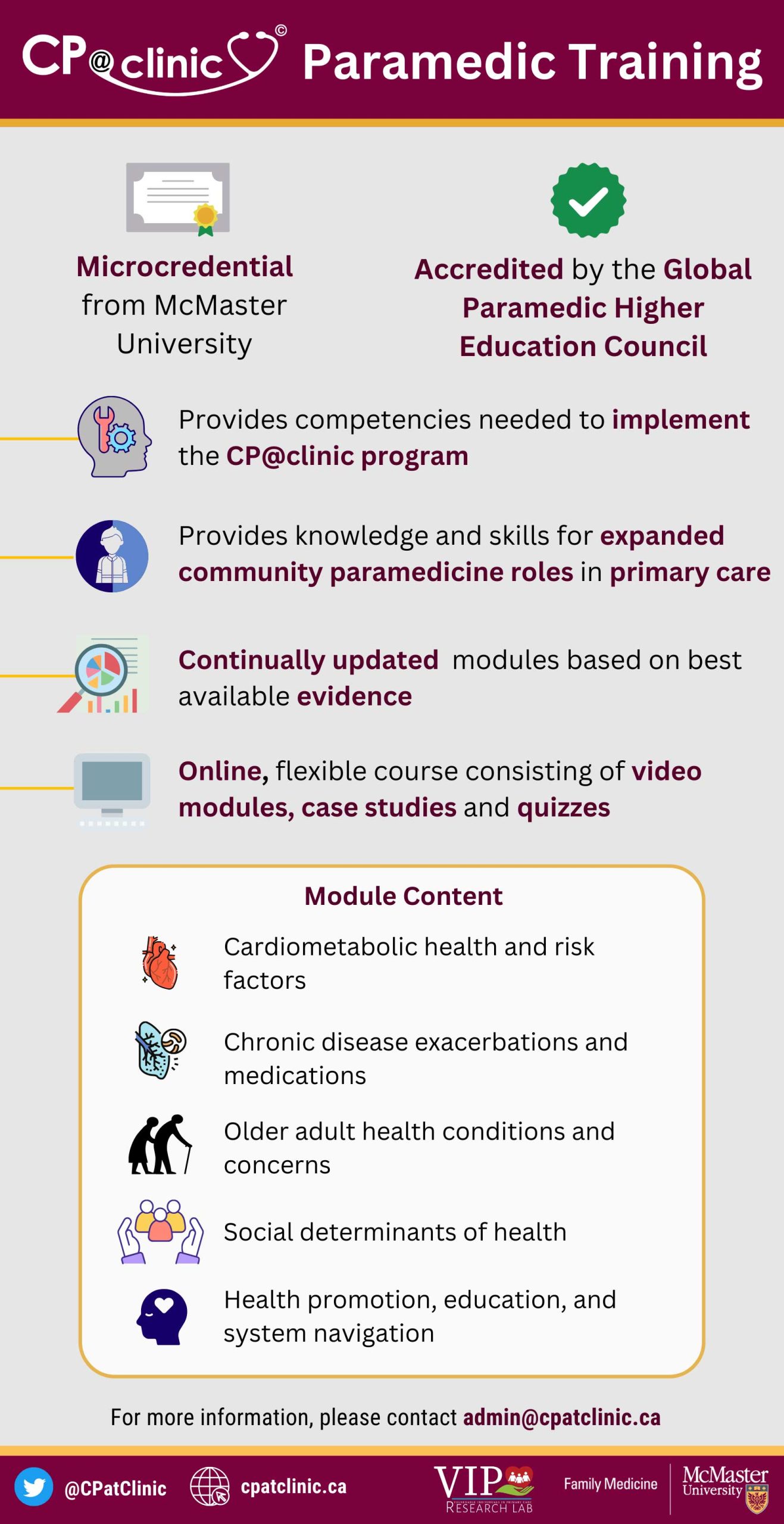
CP@clinic Paramedic Training
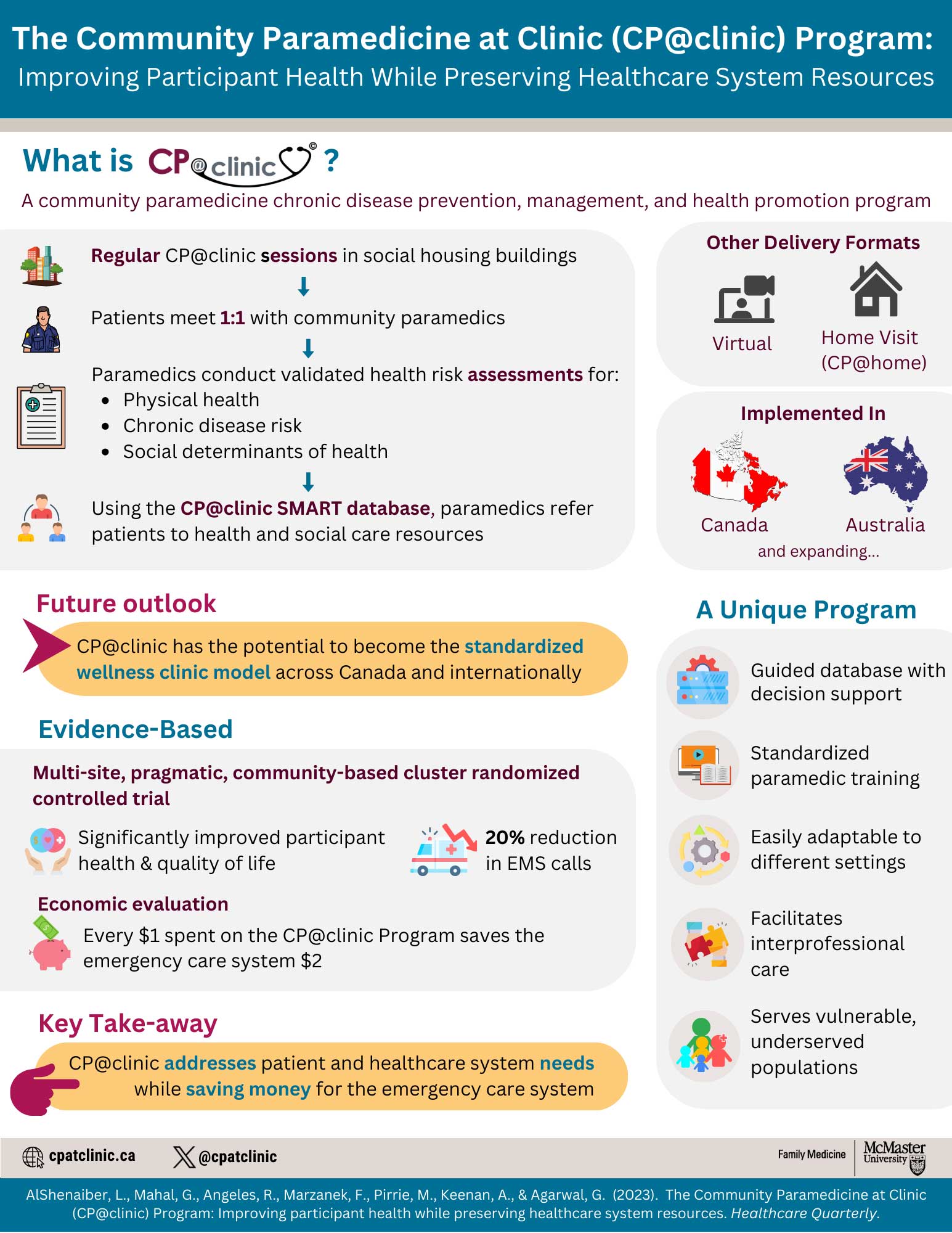
CP@clinic: Improving participant health and preserving healthcare system resources
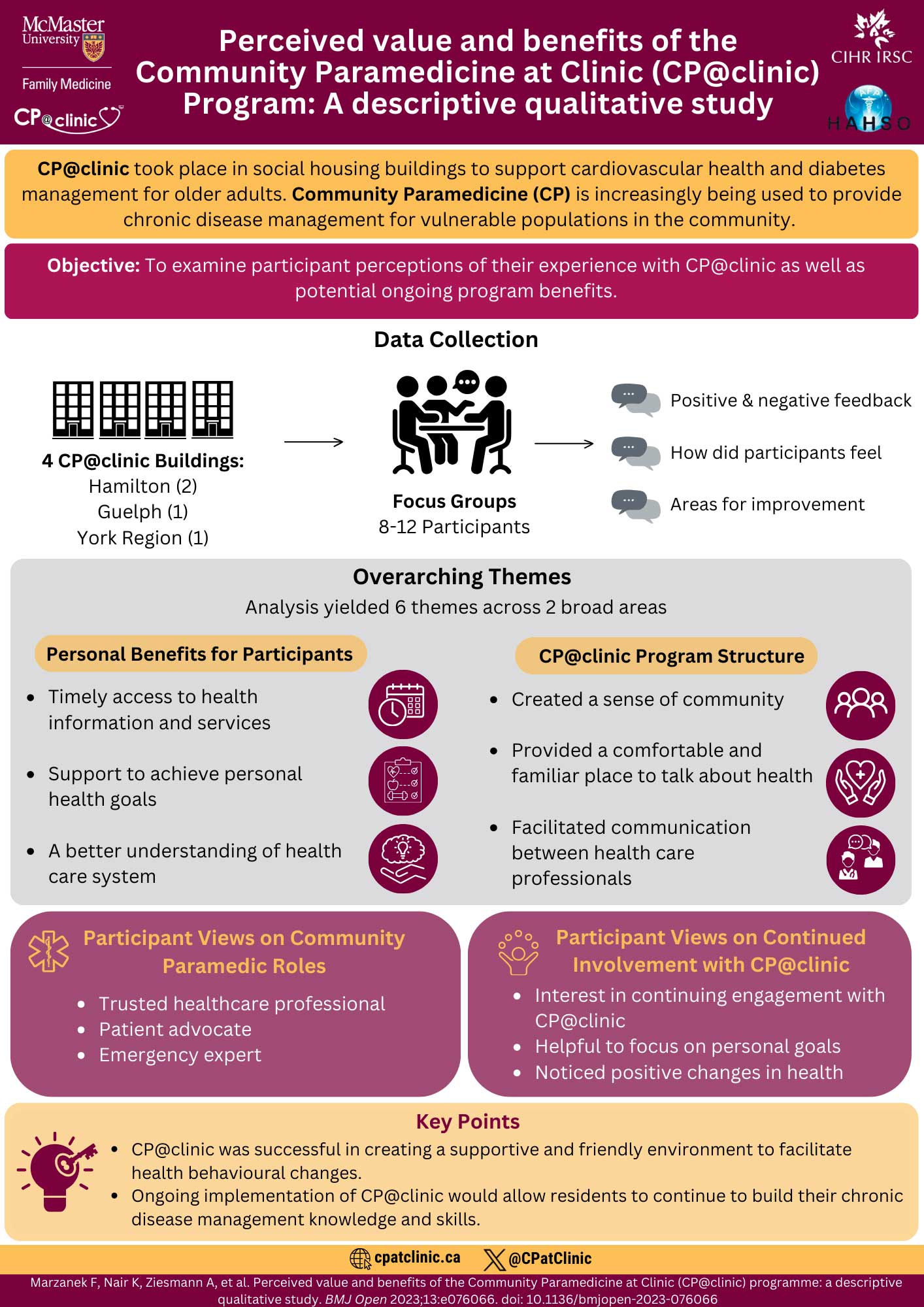
Perceived value and benefits of CP@clinic

Paramedics’ Perspectives on the Community Paramedic Role in Ontario
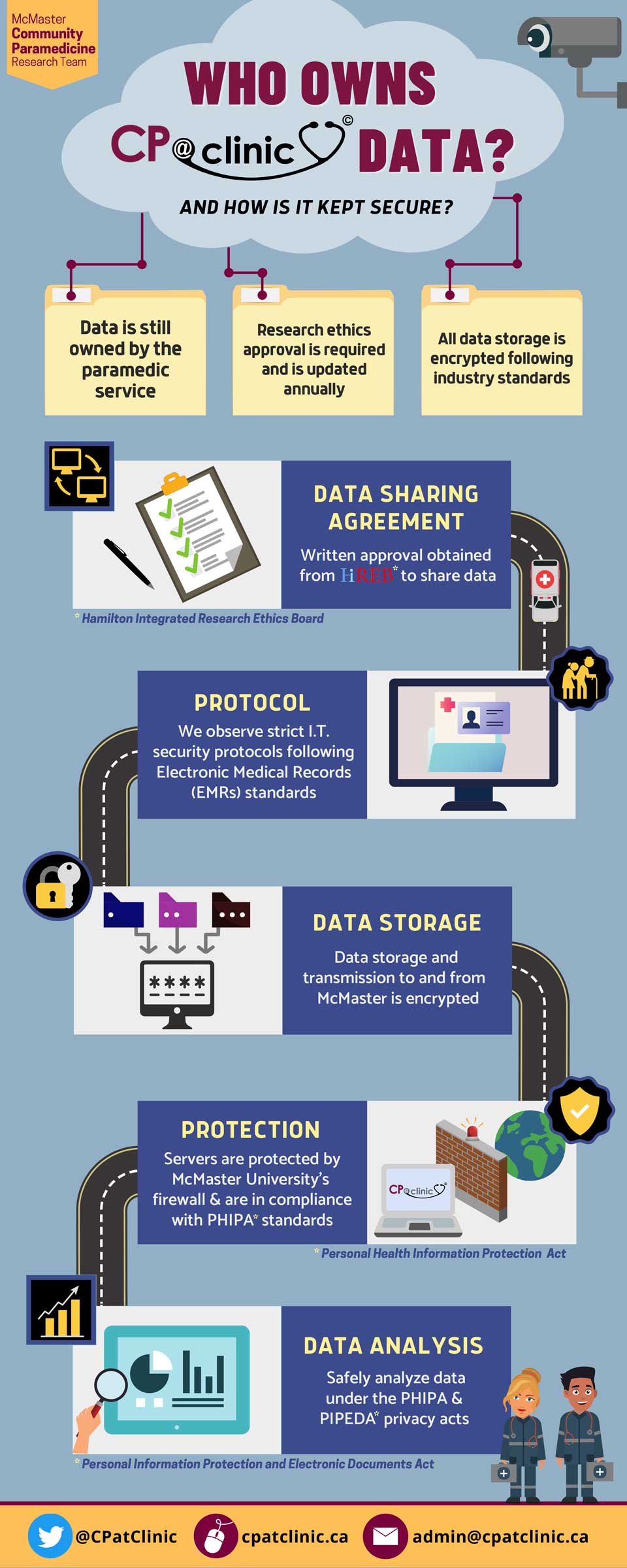
Data ownership and security for CP@clinic

Tsunami of Neglected Health Conditions

Beneath the Tip of the Pandemic Iceberg
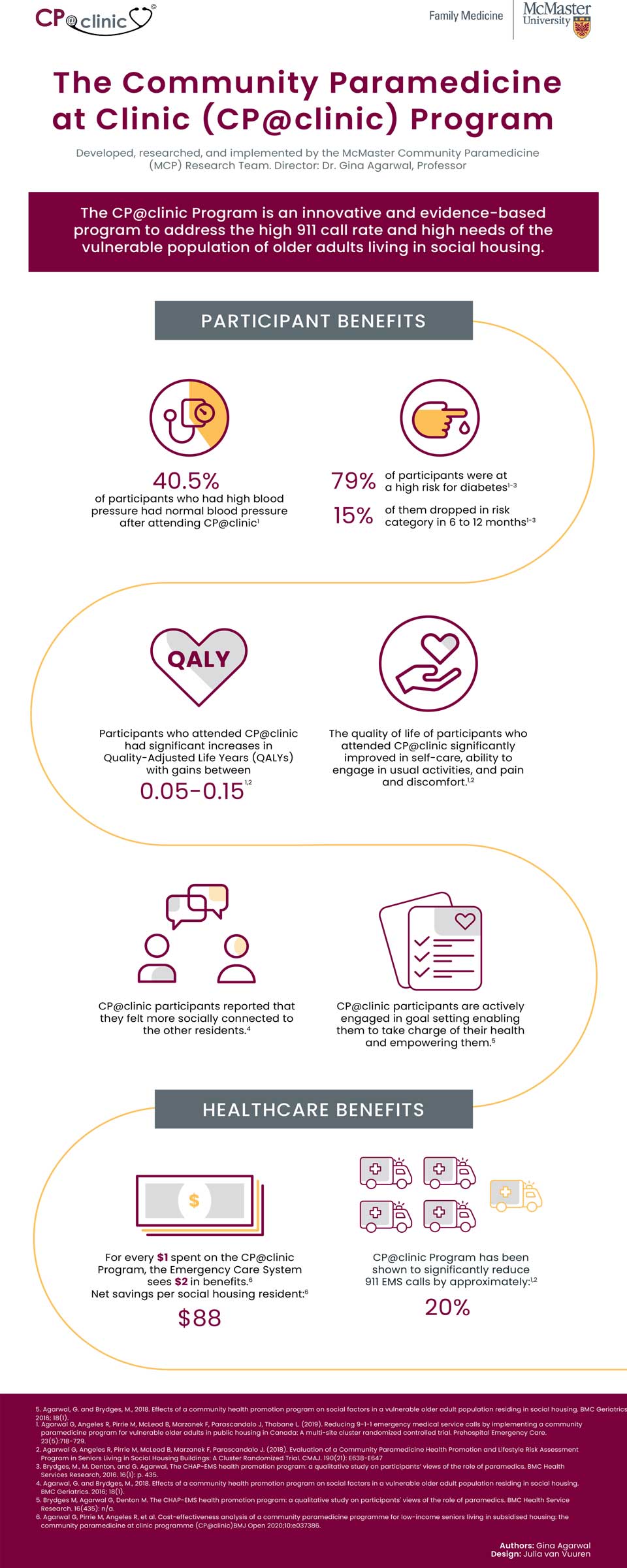
The Community Paramedicine at Clinic (CP@clinic) Program
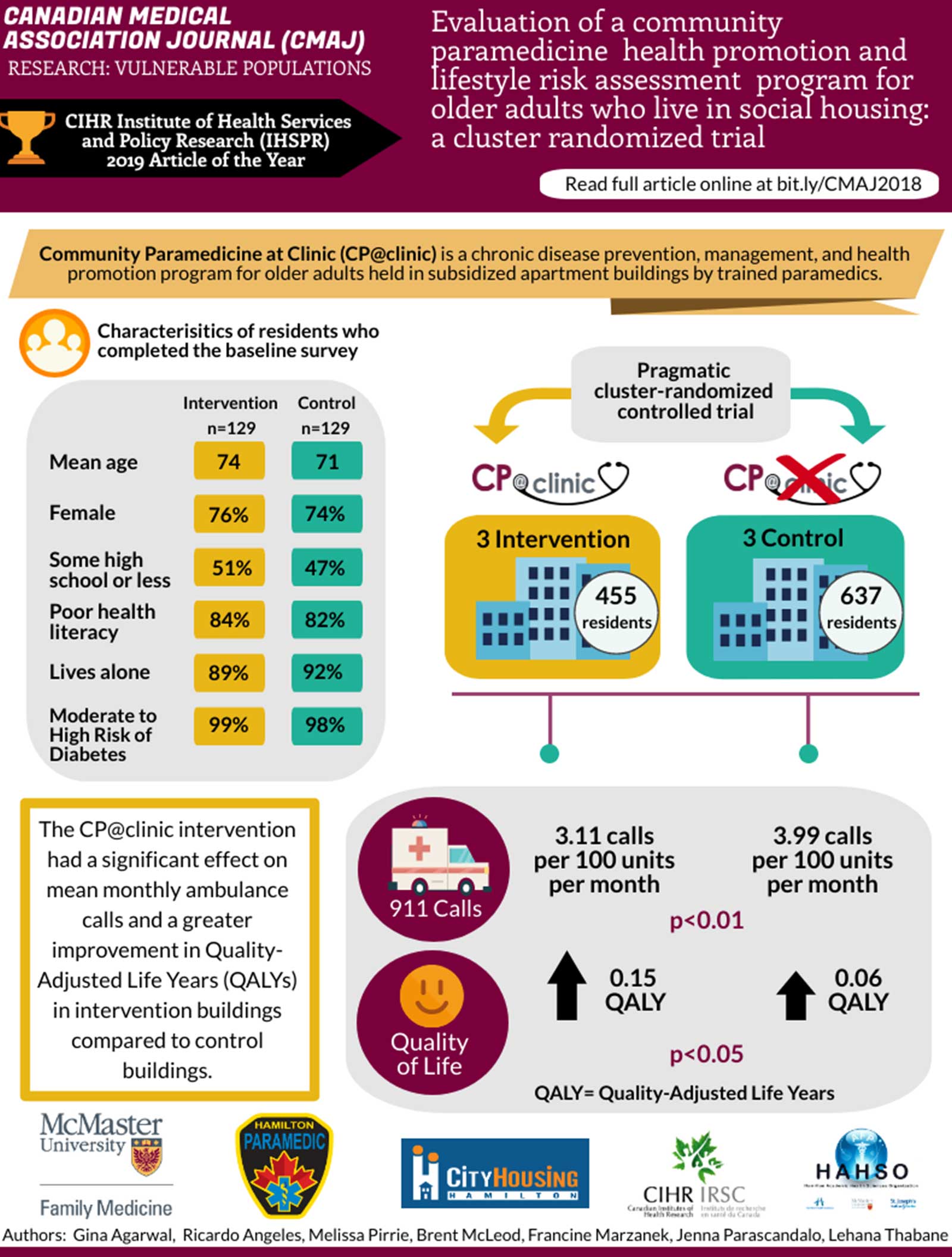
Canadian Medical Association Journal
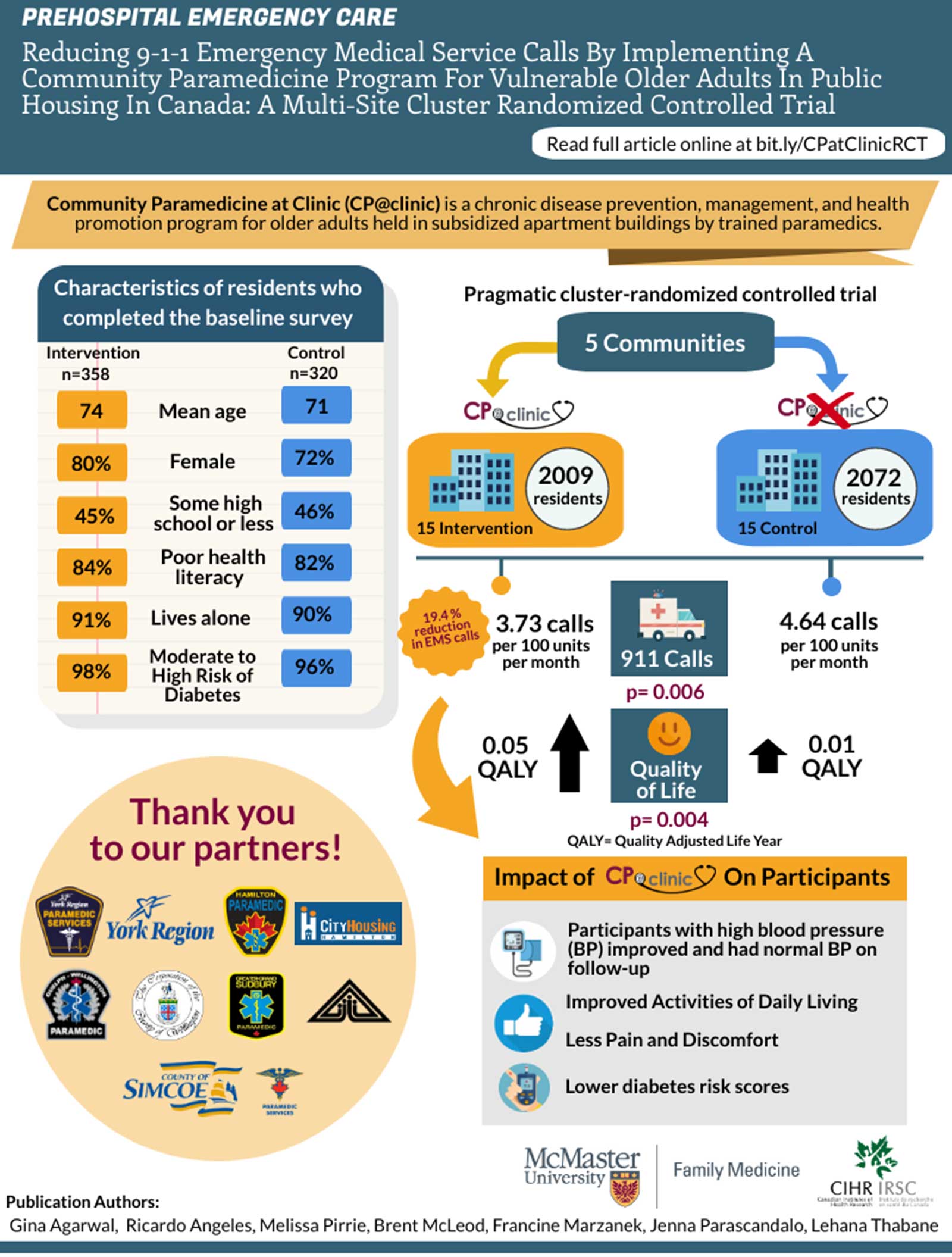
Prehospital Emergency Care
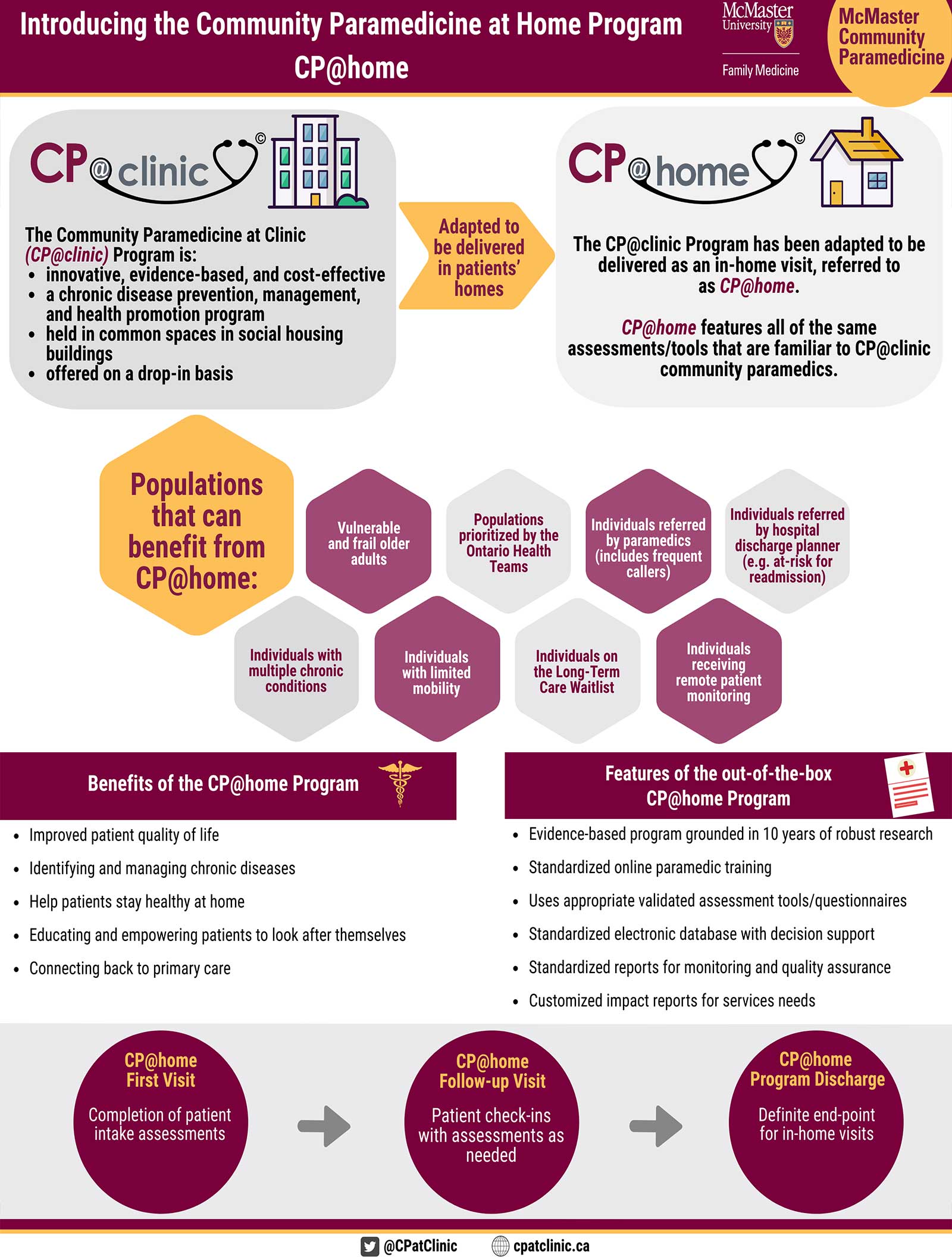
CP@home
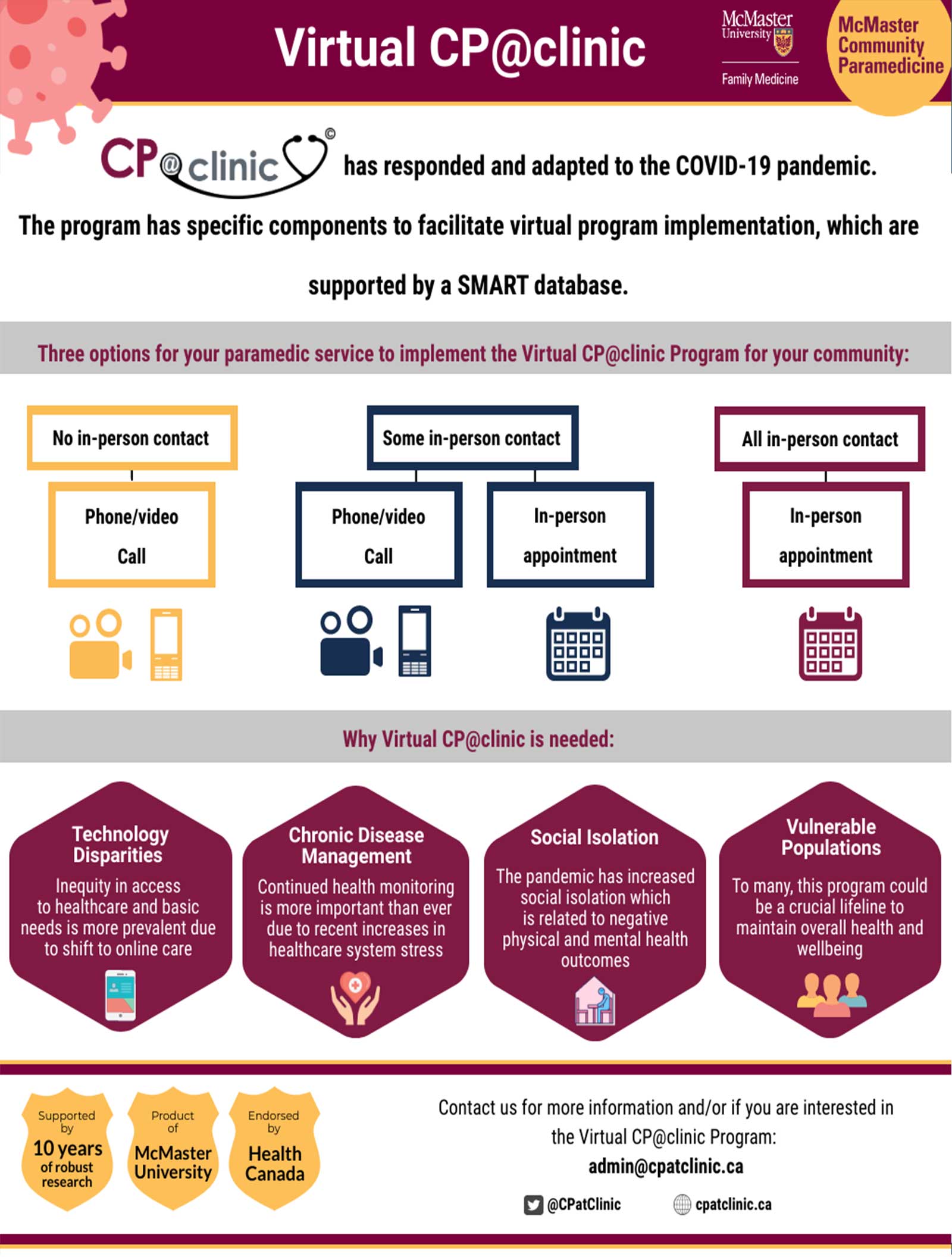
Virtual CP@clinic

Cost-effectiveness of CP@clinic

Feasibility of implementing CP@clinic with volunteers in a South Asian Population
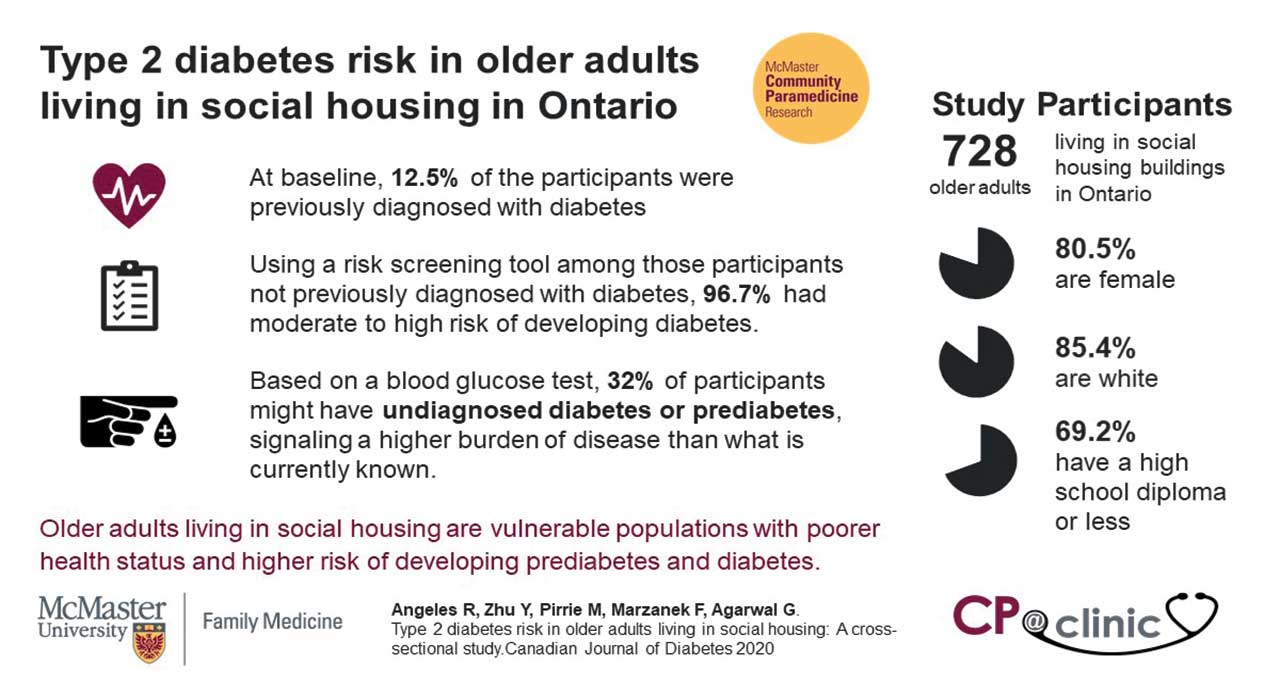
Type 2 diabetes risk in older adults living in social housing

Poverty and food insecurity of older adults living in social housing in Ontario
Health Canada Support
CP@clinic Scale-Up Supported by Health Canada



A model of care proven to reduce EMS calls — which frees up ambulances for quicker response times and may help reduce the burden on emergency departments — is expanding to sites across Canada.

Dr. Gina Agarwal and the McMaster Community Paramedicine Research Team have been awarded Health Care Policy Contribution Program (HCPCP) funding by Health Canada to expand the innovative Community Paramedicine at Clinic (CP@clinic) program with paramedic services across Canada. CP@clinic is the leading evidence-based community paramedicine wellness clinic model and has the potential to benefit communities across Canada.
CP@clinic is already well-established in Ontario implemented by 17 paramedic services in their local communities. The funding from Health Canada will allow Agarwal and her team to adapt CP@clinic to the unique needs and contexts of communities across the country and to develop the infrastructure necessary to run a sustainable program in multiple provinces.
“Working with our paramedic services partners, we have tested and improved the CP@clinic model with a broad spectrum of urban and rural communities in Ontario,” says Agarwal. “This new funding is going to help us develop locally relevant instances of the program with paramedic services across Canada.”
CP@clinic Publications
2024
Physician perspectives of the community paramedicine at clinic (CP@clinic) and my care plan app (myCP app) for older adults
Reference:
2023
Perceived value and benefits of the Community Paramedicine at Clinic (CP@clinic) programme: a descriptive qualitative study.
Reference:
Challenges in Recruiting Frequent Users of Ambulance Services for a Community Paramedic Home Visit Program.
Reference:
The Most Common Self-Reported Reasons for Calling EMS: A Cross-Sectional Survey of Frequent Callers in Ontario.
Reference:
Adapting the Community Paramedicine at Clinic (CP@clinic) program to a remote northern First Nation community: A qualitative study of community members’ and local health care providers’ views.
Reference:
2022
Paramedics’ perspectives of the community paramedic role in Ontario, Canada.
Reference:
Health knowledge and self-efficacy to make health behaviour changes: a survey of older adults living in Ontario social housing.
Reference:
Workplace violence against Emergency Health Care Workers: What Strategies do Workers use?
Reference:
Integrating community paramedicine with primary health care: A qualitative study of community paramedic views.
Reference:
2021
The effect of COVID-19 on emergency medical service call volumes and patient acuity: a cross-sectional study in Niagara, Ontario.
Reference:
Economic Analysis of Mobile Integrated Health Care Delivered by Emergency Medical Services Paramedic Teams.
Reference:
Economic Analysis of Mobile Integrated Health Care Delivered by Emergency Medical Services Paramedic Teams
Reference:
Paramedics working in general practice: a scoping review
Reference:
Reshaping healthcare delivery for elderly patients: the role of community paramedicine; a systematic review
Reference:
Social isolation in older adults residing in social housing in Ontario: a cross-sectional study.
Reference:
Time to reshape our delivery of primary care to vulnerable older adults in social housing?
Reference:
2020
Cost-effectiveness analysis of a community paramedicine programme for low-income seniors living in subsidised housing: the community paramedicine at clinic programme (CP@ clinic)
Reference:
Feasibility of implementing a community cardiovascular health promotion program with paramedics and volunteers in a South Asian population.
Reference:
Poverty and food insecurity of older adults living in social housing in Ontario: a cross-sectional study
Reference:
Risk of falls and fear of falling in older adults residing in public housing in Ontario, Canada: findings from a multisite observational study.
Reference:
Type 2 diabetes risk in older adults living in social housing: A cross-sectional study.
Reference:
Understanding Why Frequent Users of EMS Call 9-1-1: A Grounded Theory Study.
Reference:
2019
Community Paramedicine: A Systematic Review of Program Descriptions and Training.
Reference:
Reducing 9-1-1 emergency medical service calls by implementing a community paramedicine program for vulnerable older adults in public housing in Canada: A multi-site cluster randomized controlled trial.
Reference:
Social factors in frequent callers: a description of isolation, poverty, and quality of life in those calling emergency medical services frequently.
Reference:
What do community paramedics assess? An environmental scan and %content analysis of patient assessment in community paramedicine.
Reference:
2018
Assessing Health Literacy Among Older Adults Living in Subsidized Housing: A Cross Sectional Study.
Reference:
Effects of a Community Health Promotion Program on Social Factors in a Vulnerable Older Adult Population residing in Social Housing
Reference:
Evaluation of a Community Paramedicine Health Promotion and Lifestyle Risk Assessment Program in Seniors Living in Social Housing Buildings: A Cluster Randomized Trial.
Reference:
2017
Effectiveness of a community paramedic-led health assessment and education initiative in a seniors’ residence building: the Community Health Assessment Program through Emergency Medical Services (CHAP-EMS)
Reference:
2016
Examining hypertension rates, severity, knowledge, and modifiable risk factors in older adults residing in Ontario subsidised housing.
Reference:
The CHAP-EMS/CP@clinic health promotion program: a qualitative study on participants’ views of the role of paramedics.
Reference:
2015
Development of a community health and wellness pilot in a subsidised seniors’ apartment building in Hamilton, Ontario: Community Health Awareness Program delivered by Emergency Medical Services (CHAP-EMS)
Reference:
Rationale and methods of a multicentre RCT of the effectiveness of a Community Health Assessment Program with Emergency Medical Services (CHAP-EMS/CP@clinic) implemented on residents aged 55 years and older in subsidised seniors’ housing buildings in Ontario.
Reference:
2014
Effectiveness of a Community Health and Wellness Pilot in a Subsidized Seniors’ Apartment Building: CHAP-EMS/CP@clinic
Reference: